研究成果 Research Results
- TOP
- News
- Research Results
- Miniature human livers offer new platform for studying disease
Miniature human livers offer new platform for studying disease
2019.08.22Research ResultsLife & Health
Researchers from Kyushu University and the University of Pittsburgh have created miniature human livers exhibiting fatty liver disease through the genetic engineering of skin cells. These mini livers provide a new platform that more closely resembles actual human livers for better understanding the cause and progression of the disease and testing therapeutics.
“Despite promising results in mice, it is common for drugs to fail in clinical trials,” says Kazuki Takeishi, assistant professor of Liver Surgery at Kyushu University Hospital and co-lead author on the study announcing the new results in Cell Metabolism. “The problem is that mice are not humans, so we need an alternative test system that better resembles human organs.”
To create this alternative, the researchers turned to human skin cells. The researchers used a process to reprogram the skin cells into a state from which they can be converted into any kind of specialized cell. The research then changed these special cells—called induced pluripotent stem (iPS) cells—into liver cells.
Stopping here would only yield groupings of cells that reproduce some simple organ functions, so the researchers went one step further and inserted the liver cells into rat livers stripped of their own cells. There, the human liver cells grew into miniature livers containing blood vessels and other structural features (Fig. 1), although lacking some of the metabolic functions and features of true livers.
To make mini livers that exhibit fatty liver disease, the researchers first genetically engineered the starting skin cells to have a switch that could be used to suppress the gene SIRT1, which has been linked to the disease. The researchers found that chemically activating the switch to turn off the production of SIRT1 in the mini livers created from these cells resulted in features similar to those found in tissue from patients suffering from fatty liver disease (Fig. 2).
“Customized mini livers created in this way give us another research tool that I hope will accelerate the development of effective treatments for liver diseases,” states Takeishi.
For more information about this research, see “Generation of human fatty liver using custom engineered induced pluripotent stem cells with modifiable SIRT1 metabolism,” Alexandra Collin de l’Hortet, Kazuki Takeishi, Jorge Guzman-Lepe, Kazutoyo Morita, Abhinav Achreja, Branimir Popovic, Yang Wang, Kan Handa, Anjali Mittal, Noah Meurs, Ziwen Zhu, Frank Weinberg, Michael Salomon, Ira J. Fox, Chu-Xia Deng, Deepak Nagrath, and Alejandro Soto-Gutierrez, Cell Metabolism (2019), https://doi.org/10.1016/j.cmet.2019.06.017
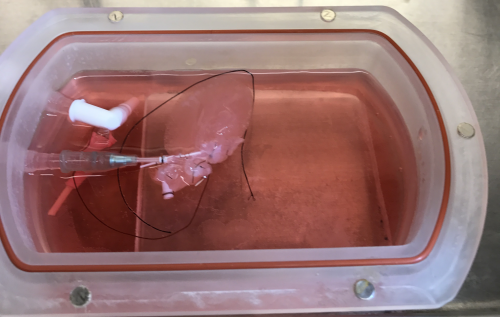
Fig. 1. Photograph of the system used to grow mini livers from human iPS cells. The inset shows one of the grown livers.
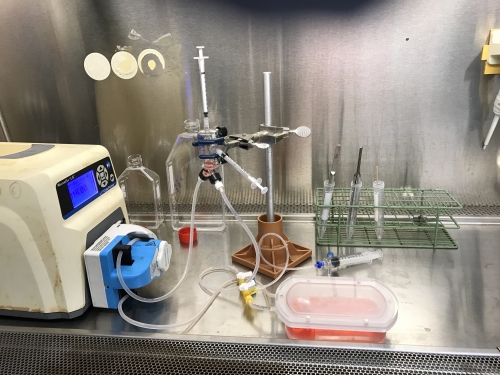
Fig. 2. Photograph of the grown livers.
Journal Reference
Generation of Human Fatty Livers Using Custom-Engineered Induced Pluripotent Stem Cells with Modifiable SIRT1 Metabolism, ,Cell Metabolism, https://doi.org/10.1016/j.cmet.2019.06.017Research-related inquiries
- TOP
- News
- Research Results
- Miniature human livers offer new platform for studying disease