研究成果 Research Results
- TOP
- News
- Research Results
- How do bad kidneys lead to heart disease? Broken cellular clocks provide new clues
How do bad kidneys lead to heart disease? Broken cellular clocks provide new clues
Researchers find how chronic kidney disease induces heart inflammation through white blood cells 2021.06.04Research ResultsLife & Health
According to the Global Burden of Disease Study 2017, close to nine percent of the global population lives with some form of chronic kidney disease, or CKD. Not only does the condition affect renal function, CKD has long been associated with increased risk of cardiovascular disease.
Now, in a new study that could aid the development of therapeutic drugs to reduce these cardiac complications, researchers led by Kyushu University have found an underlying molecular pathway that can explain how chronic kidney disease induces heart failure.
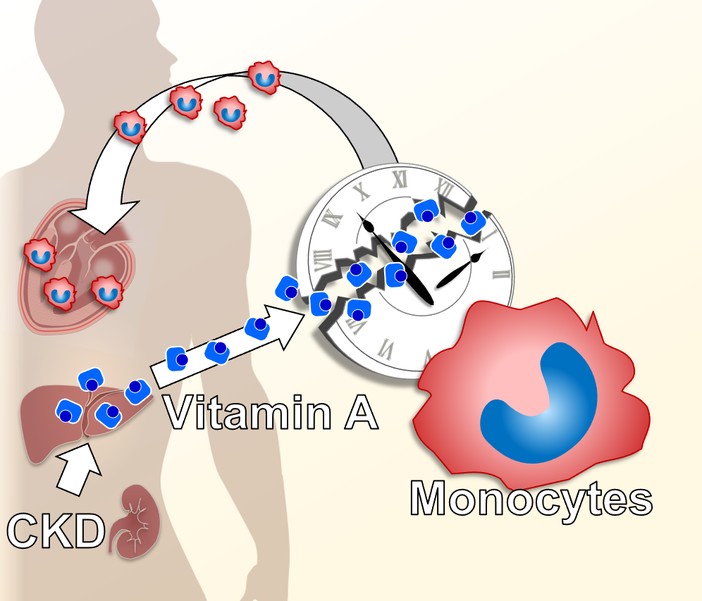
Studying mice, the researchers found that a key driver is the dysfunction of a type of white blood cell called a monocyte. The dysfunction is caused by increased levels of vitamin A and its binding protein—a common symptom of chronic kidney disease—breaking a well-known genetic pathway: the circadian clock.
The circadian clock is one of the most indispensable biological functions in living organisms. Common understanding of the pathway is that it controls our sleep patterns. However, the circadian clock plays a much larger role, affecting blood pressure, metabolic rate, and even hormone levels. In fact, nearly 10% of our genes are directly influenced by the circadian clock.
These properties made it a natural target for Shigehiro Ohdo, professor of Kyushu University’s Faculty of Pharmaceutical Sciences, and his team for investigating the causes of chronic kidney disease-induced heart inflammation and fibrosis.
“We found that mice with a mutated Clock gene—one of the main regulators of the circadian clock—have decreased symptoms of heart problems related to chronic kidney disease, despite having high blood pressure,” explains Yuya Yoshida, one of the first authors of the study published in the journal Nature Communications.
To search for the underlying cause of this protective effect, the team looked for abnormalities in genes that connect Clock and kidney dysfunction.
“Our investigation led us to find that a protein called 'G protein-coupled receptor 68,' or GPR68, produced in monocytes was playing a key role. GPR68 is known to increase the production of proteins that cause inflammation, and more importantly, it is regulated by the Clock gene,” states Naoya Matsunaga, another author of the study.
One sign of kidney dysfunction is elevated levels of vitamin A and its binding protein, two molecules that are usually carefully controlled. The researchers found that this elevation disrupts the normal activity of the circadian clock in monocytes, which in turn over-express GPR68.
These high-GPR68-expressing monocytes then infiltrate the heart and cause inflammation and fibrosis. This explains why mice with defective Clock genes have less severe CKD-induced heart problems: there is no Clock gene to produce GPR68.
“Our study reveals a previously unknown role of monocytic Clock genes in CKD-induced heart failure,” concludes Ohdo. “The findings will help us develop therapeutic drugs such as ones targeting GPR68. We also can investigate better treatments for abnormal vitamin A accumulation in the blood.”
###
For more information about this research, see “Alteration of circadian machinery in monocytes underlies chronic kidney disease-associated cardiac inflammation and fibrosis,” Yuya Yoshida, Naoya Matsunaga, Takaharu Nakao, Kengo Hamamura, Hideaki Kondo, Tomomi Ide, Hiroyuki Tsutsui, Akito Tsuruta, Masayuki Kurogi, Michio Nakaya, Hitoshi Kurose, Satoru Koyanagi, and Shigehiro Ohdo, Nature Communications (2021). https://doi.org/10.1038/s41467-021-23050-x
This release is also available in Japanese.
Research-related inquiries
Shigehiro Ohdo, Professor
Department of Pharmaceutical Health Care and Sciences, Faculty of Pharmaceutical Sciences
Contact information can also be found in the full release.
- TOP
- News
- Research Results
- How do bad kidneys lead to heart disease? Broken cellular clocks provide new clues